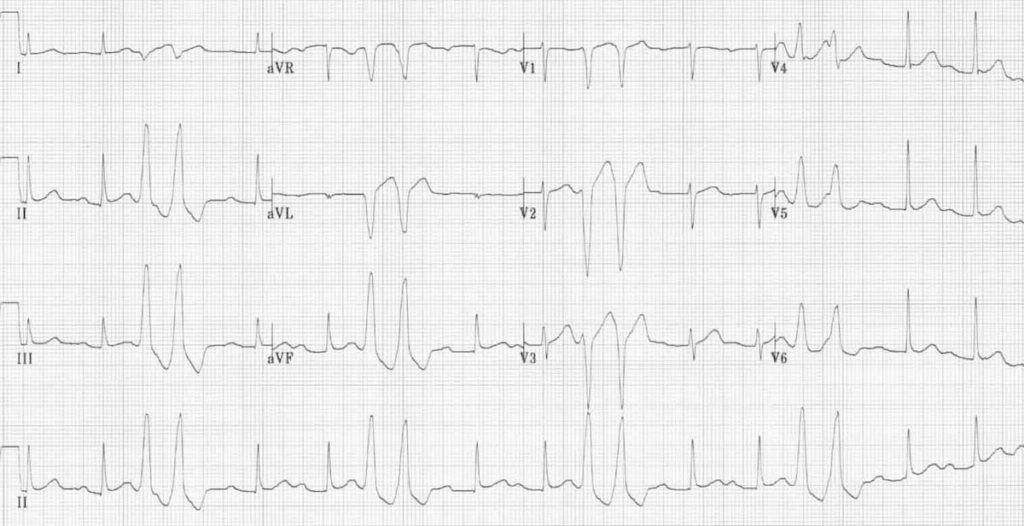
Occasional Pvc
PVCs may indicate the presence of underlying heart disease. If a patient has NO significant underlying heart disease, PVCs are probably not dangerous. Most “anti-arrhythmic” drugs are relatively poor at treating PVCs (though they often reduce their frequency.) and can make dangerous arrhythmias more likely.
- In some rare individuals, extremely frequent PVCs are now thought to be responsible for producing cardiomyopathy (weak heart muscle). As a result, if unexplained cardiomyopathy is found in the presence of very frequent PVCs, it may be helpful to treat the PVCs to see if the cardiomyopathy improves.
- PVCs often occur in repeating patterns: Bigeminy — every other beat is a PVC. Trigeminy — every third beat is a PVC. Quadrigeminy — every fourth beat is a PVC. Couplet — two consecutive PVCs. NSVT — three-thirty consecutive PVCs (see below).

Ventricular tachycardia is a fast heart rate, anything over the normal 100 beats per minute, which starts in the lower chambers of the heart, the ventricles. It causes the ventricles to contract before they have had a chance to completely fill with blood, impairing blood flow to the body.
Normal Pvcs Per Day
Premature Ventricular Contractions (PVCs) are single beats originating from the lower chambers. Any time there is more than 3 beats in succession this is defined as ventricular tachycardia.
Most of the time ventricular tachycardia occurs in people with underlying heart abnormalities. Sometimes in can occur in structurally normal hearts. In these patients the origin is usually the right ventricular outflow tract (RVOT). The route the blood flows from the right ventricle to the lungs. In other patiens, such as those who have had a heart attack, the scar from the heart attack creates a milieu of intact heart muscle and scar that predisposes to VT.
Ventricular Tachycardia (VT) and Premature Ventricular Contractions (PVCs)
This is a serious disorder and requires prompt treatment. It may evolve into the ventricular fibrillation. In this life-threatening condition, the ventricles quiver, pumping very little blood out of the heart. Ventricular fibrillation is the primary cause of sudden cardiac death. If normal rhythm is not restored within 3-5 minutes, the heart and brain will be damaged, and the patient will die. Ventricular tachycardia and ventricular fibrillation can be converted into normal rhythm with a controlled electrical shock from a defibrillator.
Regular treatment of ventricular tachycardia include medications to slow the heart rate. High-risk patients are treated with an implantable cardioverter-defibrillator (ICD). [Learn more]
Catheter ablation is the treatment of choice in patients with RVOT VT. Catheter ablation can be used in patients with scar to prevent receiving numerous shocks from an ICD.
Ablation of ventricular tachycardia in a patient with an old heart attack. The target for ablation are islands of live tissue within the scar. These islands cause a circuit for the ventricular tachycardia. The ablation electrically isolates these live islands of live tissue within the scar from healhty tissue.

Menopause goes hand-in-hand with many annoying symptoms. Some are well known (hot flashes, night sweats, mood swings and fatigue, to name a few), while some are more uncommon and lesser known (burning mouth syndrome, crawling sensation on skin or electric shocks). But did you know that perimenopause is rife with its own pesky traits as well?
There is a symptom that women may be experiencing but they may not initially associate it with perimenopause or menopause. Oh, how I wish I had known about this fright-inducing symptom before I had my own personal meltdown.
September 19, 2014. It was a mild, sunny day in Stamford, Connecticut. I was excited about the day ahead of me. I had recently turned 51. As far as I knew, I hadn’t been experiencing any obvious symptoms of menopause. Then again, I wasn’t exactly privy to what the symptoms were, aside from hot flashes. I was effectively in the dark, having never had that crucial conversation with my mother, my older sisters, my gynecologist or anyone else.
Life was relatively normal for me except for one odd thing. The previous week, I had been experiencing an odd fluttering sensation in my chest, but I ignored the symptoms. I didn’t want to be hypochondriacal, so I ignored it.
On that unseasonably warm Sunday, my focus was on my destination. Gospel music played softly through the car speakers as I cruised up the Merritt Parkway on my way to Bridgeport for brunch. That’s when it happened.
It began as a flutter in my chest, then escalated to so much more. I didn’t know what was happening to me. Was I having a heart attack? A stroke? Panic washed over my body as my arms began to tingle, and a prickling sensation assaulted my face. Breathing became difficult, each breath a labor of my perceived survival. The pounding in my chest was relentless.
My mind went numb. I veered off the Parkway, swerving around the corner as alarm and confusion set in. I frantically called my husband because I thought I was dying. I was sure of it. It didn’t occur to me to dial 911.
In full-blown panic mode, I began to flag down cars. A nurse driving past spotted me, stopped, called 911, spoke with my husband to keep him apprised of my condition and stayed with me until the ambulance arrived. I was transported to the hospital – my first overnight hospital stay . . . ever.
Over the next two days, I was poked, prodded, stress tested, interrogated, second-guessed and awakened every four hours – no one had a clue what was wrong with me. I was released from the hospital with a diagnosis of “Anxiety Attack.”
Bullshit.
When I arrived back home – disillusioned with the medical community and annoyed at being labeled an anxiety case – I turned to Google. I began to research my symptoms. My virtual legwork paid off. I came across an article in O, The Oprah Magazine. The article had a profound impact on me because 1) it was penned by Oprah, and 2) I saw myself in her words.
Now, here is where Oprah and I have simpatico – she was experiencing the same symptoms that plagued me. Oprah awoke with such intense heart palpitations, her heart was pounding like it was about to beat out of her chest. She, too, thought she was knocking at death’s door. And this shared scare – this over-stimulation of the heart resulting in an increasing heart rate – is related to diminished estrogen levels.
After further research and a subsequent visit to a menopause specialist, I was able to put a name to what happened to me: Premature Ventricular Contractions (PVCs).
The Mayo Clinic defines PVCs as “extra heartbeats that begin in one of your heart’s two lower pumping chambers (ventricles).” PVCs are generally regarded as non-threatening, however, frequent PVCs may increase the risk of developing a more serious arrhythmia or cardiomyopathy.
Time Marches On
I continued to experience PVCs for the next couple of weeks. However, knowing exactly what it was that I was experiencing went a long way in allaying fears of my immediate demise.
Today, I still have the occasional PVC episode, but I do what I can to manage the occurrences. I’ve cut down drastically on my sugar intake and processed foods in favor of whole foods. When I’m in the throes of a PVC onset, mindful breathing has helped to calm me and relax my breathing.
Perimenopause and menopause can definitely be problematic. While a lot of what occurs during this time is bothersome, there are also some positive aspects to be considered: period-free, shrinking fibroids, or no pregnancy worries, among others.
Unfortunately, with perimenopause and menopause comes a significant drop in estrogen. When that occurs, our bodies respond (and not in the way we want). Sadly, that triggered response doesn’t result in silky flowing hair, a miraculously perky bosom or an increased metabolism. Simply put, perimenopause sucks. And then comes menopause – this is that delightful stage where women are blessed with the amazing opportunity to jump out of the frying pan and take up residence in the fiery pit of Lady Hell (yeah, I’m looking at you, hot flashes).
Take heart, though, ladies. The picture is not as bleak as it seems. Palpitations aren’t necessarily the end of the world. Having said that, if you experience palpitations, don’t ignore that fluttering and pounding sensation. Schedule an appointment with your doctor so that other, more serious ailments can be ruled out, such as atrial fibrillation. (The risk of heart disease increases for menopausal women, so be mindful of this).
Occasional Pvcs
Your palpitations could be a symptom of perimenopause . . . or not.
If your gynecologist isn’t providing you with the answers you need, perhaps it’s time to turn to a menopause specialist. To find a menopause practitioner near you, visit Menopause.org.
Have you ever experienced PVCs in peri- or menopause? Let’s discuss it in the comments.
This article originally appeared on Pepper&Wits.